Medical Only Adjuster Resume
Headline : As a Medical Only Adjuster, responsible for Accepting new cases from customers, Ensuring that cases are handled in a timely manner while adhering to company guidelines, ensuring that all documents are filed properly, including case notes and insurance forms, and also Providing customer service when needed.
Skills : Office Administration, Office Equipment, Workers Compensation, Workers Compensation.
Description :
- Able to verify lost time, waiting periods and wage loss.
- Processed benefits daily to avoid penalty and interest.
- Processed manual bill payments.
- Handled bill/claim calls.
- Maintained current file documentation including all incoming medical reports Established contact with employer to confirm no lost time claims and no .
- Handled and maintained workman's comp medical only claims, enter medical notes, process bills, call providers, claimants.
- Managed Medical until injured worker is MMI or file reaches qualified status for Loss Time file.

Experience
5-7 Years

Level
Executive

Education
High School Or Equivalent
Medical Only Adjuster Resume
Summary : As a Medical Only Adjuster, responsible for Providing guidance to adjusters for all aspects of the process, Conducting quality assurance reviews on adjusters' work, Identifying opportunities for improvement in the claims resolution process, Working with the field to identify opportunities for improvement in the claims resolution process, Working with field to identify new business development opportunities.
Skills : Microsoft Office, Medisys Software.
Description :
- Maintained established treatment guidelines for workers' compensation diagnostics and surgeries and ensure physicians are aware of current treatment guidelines utilized by the various carriers.
- Set or recommended reserves based on results of claim investigation.
- May provided interaction with insureds, agents, claimants, attorneys, and other service providers.
- Conducted in-depth interviews and/or scene inspections.
- Worked closely with physicians to coordinate causation letters and appeals when compensability is disputed.
- Assisted in ensuring the timely payment of benefits, medical and vendor bills and processed state required filings.
- Maintained effective and ongoing communication within the office and with outside parties.

Experience
7-10 Years

Level
Management

Education
BS In Finance
Medical Only Adjuster Resume
Objective : Medical Only Adjuster is responsible for Creating a claim file for each case and gathering the necessary information to process the claim, Investigating the claim to determine the cause and potential solutions, and Following up with the client or patient to ensure they are satisfied with the resolution of their claim.
Skills : Interpersonal Skills Medical Skills, Coordinating Skills.
Description :
- Responsible for managing all aspects of each claim and maintaining a high level of productivity, confidentiality and customer service.
- Implemented and coordinated the most effective management techniques to mitigate loss and expense payments.
- Reserved and expensed authority levels are moderate.
- Worked with the Special Investigations Unit, where appropriate.
- Knowledged of medical terminology.
- Cultivated an environment of teamwork and collaboration
- Operated with latitude for un-reviewed action or decision.

Experience
2-5 Years

Level
Executive

Education
BA In Psychology
Medical Claims Adjuster Resume
Objective : Dynamic Medical Claims Adjuster with 2 years of focused experience in evaluating and processing claims. Skilled in analyzing policy coverage and ensuring compliance with industry standards. Adept at providing exceptional customer service while managing complex claim cases. Eager to contribute valuable insights and support to a dedicated team in the healthcare insurance sector.
Skills : Data Analysis, Problem Solving, Negotiation Skills, Insurance Regulations
Description :
- Utilized strong analytical skills to assess complex claims and ensure accurate processing.
- Communicated effectively with policyholders, attorneys, and healthcare providers to resolve claims issues.
- Monitored claims for compliance with state regulations and company policies.
- Developed and maintained comprehensive knowledge of healthcare insurance products and services.
- Provided timely updates to stakeholders regarding claim status and outcomes.
- Collaborated with team members to enhance overall claims processing efficiency.
- Leveraged technology to track and manage claims, ensuring data integrity.

Experience
0-2 Years

Level
Entry Level

Education
AAS-HCA
Junior Medical Claims Adjuster
Resume
Objective : Enthusiastic Medical Claims Adjuster with 2 years of hands-on experience in evaluating and processing medical claims. Proficient in analyzing policy details and ensuring adherence to regulations. Committed to delivering outstanding customer service while effectively managing intricate claims. Ready to enhance team performance and contribute to the success of a healthcare insurance organization.
Skills : Customer Service Excellence, Risk Assessment, Conflict Resolution, Team Collaboration, Report Writing
Description :
- Review and analyze medical claims for accuracy and compliance with policies.
- Verified coverage by examining contracts and policy documents.
- Reviewed medical documents and claims history to ensure accuracy.
- Trained on client-level business rules to facilitate appropriate claims decisions.
- Negotiated pricing with vendors to achieve favorable claim settlements.
- Issued payments and resolved escalated claims inquiries.
- Managed multiple medical claims simultaneously, addressing various issues effectively.

Experience
0-2 Years

Level
Junior

Education
B.S. Health Admin.
Medical Claims Adjuster Resume
Headline : Accomplished Medical Claims Adjuster with 7 years of extensive experience in evaluating and processing complex claims. Expert in policy analysis, compliance, and claims adjudication. Known for delivering exceptional client service while efficiently managing high-volume caseloads. Committed to enhancing operational efficiency and supporting team success within the healthcare insurance landscape.
Skills : Process Improvement, Workflow Management, Insurance Claims Review, Statistical Analysis, Database Management, Claims Auditing
Description :
- Evaluated insurance policies and processed claims to ensure compliance with industry regulations.
- Analyzed medical records and billing statements to authorize appropriate payments within coverage limits.
- Collaborated with healthcare providers to resolve discrepancies and ensure accurate claims processing.
- Provided expert guidance on claims procedures, enhancing departmental efficiency.
- Conducted thorough investigations of complex claims to mitigate risk and prevent fraud.
- Maintained detailed records of claims, ensuring accuracy and compliance throughout the process.
- Utilized claims management software to streamline operations and improve reporting accuracy.

Experience
5-7 Years

Level
Senior

Education
B.S. Health Admin.
Senior Medical Claims Adjuster
Resume
Summary : Results-oriented Senior Medical Claims Adjuster with over 10 years of expertise in claims processing and adjudication. Proficient in analyzing complex policy coverage and ensuring compliance with regulatory standards. Recognized for exceptional problem-solving skills and delivering outstanding customer support while managing high-volume claims efficiently. Committed to driving operational excellence in the healthcare insurance industry.
Skills : Technical Proficiency, Case Management, Regulatory Compliance, Communication Skills, Time Management, Critical Thinking
Description :
- Evaluated and processed medical claims in accordance with plan documentation and regulatory guidelines.
- Conducted thorough audits to ensure compliance and accuracy in claims processing.
- Interpreted complex policy documents and medical terminology to facilitate accurate claims adjudication.
- Collaborated with medical professionals to clarify claim details and resolve discrepancies.
- Managed high-dollar claims and prioritized tasks based on daily operational reports.
- Maintained customer service logs with a turnaround time of 5 days, ensuring prompt responses.
- Ensured adherence to state laws and internal policies throughout the claims process.

Experience
7-10 Years

Level
Management

Education
B.S. Health Admin.
Medical Claims Adjuster Resume
Objective : Motivated Medical Claims Adjuster with 2 years of experience in claims evaluation and processing. Proficient in policy analysis and compliance, with a strong focus on delivering exceptional service to clients. Skilled at resolving complex claims issues and enhancing operational efficiency within healthcare insurance teams.
Skills : Claims Pre-authorization, Workers' Compensation Analysis, Documentation Skills, Analytical Skills, Multi-tasking, Adaptability
Description :
- Executed thorough coding of inpatient charts, maintaining high accuracy and efficiency.
- Completed claims paperwork and documentation with precision, ensuring compliance with regulations.
- Coded and billed medical claims for hospitals and outpatient facilities, optimizing reimbursement.
- Conducted research on new diagnoses and procedures to enhance coding knowledge.
- Identified and corrected inconsistencies in medical documentation, ensuring accuracy in claims.
- Addressed provider inquiries, delivering detailed responses and support.
- Reviewed outpatient medical records, analyzing diagnostic and treatment coding.

Experience
0-2 Years

Level
Entry Level

Education
AAS HIT
Associate Medical Claims Adjuster
Resume
Objective : Dedicated Medical Claims Adjuster with 2 years of experience in evaluating and processing medical claims efficiently. Expertise in analyzing insurance policies and ensuring compliance with regulations. Proven ability to deliver superior customer service while managing complex claims. Looking to leverage my skills to support a dynamic team in the healthcare insurance industry.
Skills : Policy Interpretation, Fraud Detection, Record Keeping, Billing Procedures
Description :
- Processed incoming medical claims, determining client benefit coverage while ensuring adherence to Fair Claim Practice Guidelines.
- Provided outstanding service to customers, effectively assessing and resolving claims associated with losses.
- Conducted thorough coverage and liability investigations, applying appropriate negligence guidelines.
- Reviewed necessary medical documentation to set and monitor reserves for accuracy.
- Identified potential fraud indicators and subrogation opportunities throughout the claims lifecycle.
- Calculated proper compensation amounts, processed claims payments, and coordinated benefits including Medicaid.
- Ensure timely processing of claims to meet company standards.

Experience
0-2 Years

Level
Fresher

Education
B.S. Health Admin
Medical Claims Adjuster Resume
Summary : Detail-oriented Medical Claims Adjuster with over 5 years of experience in evaluating and processing medical claims. Proficient in analyzing medical records, verifying coverage, and ensuring compliance with regulations. Strong communication skills and a commitment to resolving claims efficiently while maintaining high customer satisfaction. Adept at collaborating with healthcare providers and insurance teams to streamline processes.
Skills : Strong Analytical Skills With Attention To Detail, Decision Making, Client Relations, Empathy, Organizational Skills, Work Ethic
Description :
- Managed first-party medical claims, ensuring timely resolution and compliance.
- Provided comprehensive explanations of medical insurance benefits to insured individuals and their representatives.
- Reviewed and issued payments to insureds and medical providers after thorough claim investigation.
- Promoted three times during tenure at State Farm Insurance for outstanding performance.
- Monitored workflow quality, implementing changes to meet Service Level Agreements.
- Conducted detailed reviews of medical coding, fee schedules, and reimbursement methodologies.
- Collaborated with legal teams and medical professionals to facilitate complex claim resolutions.

Experience
10+ Years

Level
Senior

Education
BSHA
Assistant Medical Claims Adjuster
Resume
Objective : Proficient Medical Claims Adjuster with 2 years of experience in claim evaluation and processing. Demonstrated expertise in analyzing policy details and ensuring compliance with industry standards. Strong focus on delivering high-quality customer service while effectively managing complex claims. Eager to apply analytical skills to support a dynamic healthcare insurance team.
Skills : Icd-10 Coding, Cpt And Hcpcs Level Ii Coding, Microsoft Office Suite, Advanced Excel Skills, Presentation Skills, Claims Processing
Description :
- Evaluated and adjusted medical and hospital claims for healthcare providers across multiple states, ensuring compliance with regulations.
- Analyzed medical supply equipment claims for reimbursement, collaborating with suppliers for accurate processing.
- Investigated suspicious claims to identify potential fraud, maintaining integrity in the claims process.
- Assessed all evidence to facilitate positive outcomes for client claims, enhancing customer satisfaction.
- Conducted follow-ups on flagged claims initiated by claims representatives, ensuring thorough evaluations.
- Reviewed and substantiated legitimate claims, denying unjustified claims based on policy guidelines.
- Maintained detailed records of all claims processed to support audits and compliance checks.

Experience
0-2 Years

Level
Fresher

Education
B.S. in HA
Medical Claims Adjuster Resume
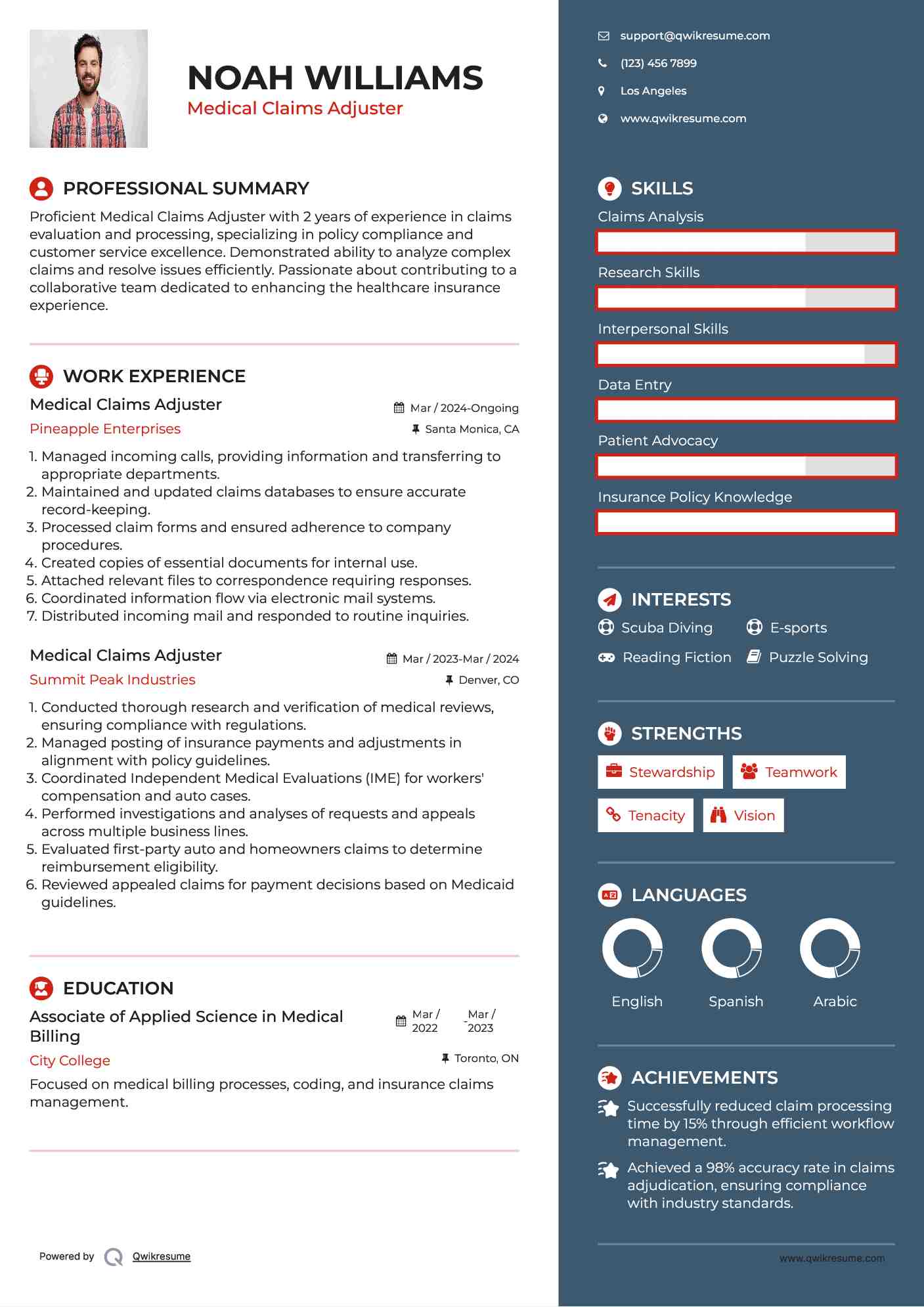
Objective : Proficient Medical Claims Adjuster with 2 years of experience in claims evaluation and processing, specializing in policy compliance and customer service excellence. Demonstrated ability to analyze complex claims and resolve issues efficiently. Passionate about contributing to a collaborative team dedicated to enhancing the healthcare insurance experience.
Skills : Claims Analysis, Research Skills, Interpersonal Skills, Data Entry, Patient Advocacy, Insurance Policy Knowledge
Description :
- Managed incoming calls, providing information and transferring to appropriate departments.
- Maintained and updated claims databases to ensure accurate record-keeping.
- Processed claim forms and ensured adherence to company procedures.
- Created copies of essential documents for internal use.
- Attached relevant files to correspondence requiring responses.
- Coordinated information flow via electronic mail systems.
- Distributed incoming mail and responded to routine inquiries.

Experience
0-2 Years

Level
Entry Level

Education
AAS
Medical Claims Adjuster Resume
Headline : Results-driven Medical Claims Adjuster with 7 years of comprehensive experience in processing and adjudicating complex medical claims. Specializes in policy analysis, regulatory compliance, and optimizing claims workflows. Recognized for delivering exceptional customer service and effectively managing high-volume caseloads. Dedicated to enhancing operational efficiency and fostering team success in healthcare insurance.
Skills : Customer Service, Medical Terminology, Claims Review, Medical Coding, Attention To Detail
Description :
- Evaluated and processed a high volume of medical claims, ensuring compliance with industry regulations.
- Conducted thorough reviews of insurance policies to verify coverage for health services.
- Analyzed Medicaid claims against benefit plan designs to enhance processing efficiency.
- Maintained detailed logs of all claims and communications to ensure accuracy and transparency.
- Resolved customer inquiries and issues related to claims status and eligibility.
- Collaborated with healthcare providers to clarify claims information and expedite processes.
- Utilized data analysis to identify trends and improve claims management processes.

Experience
5-7 Years

Level
Management

Education
B.S. in HCA